Knee Bursitis
Knee Bursitis
Background and Etiology
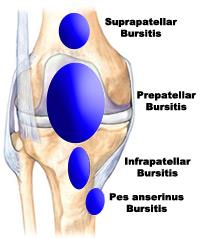
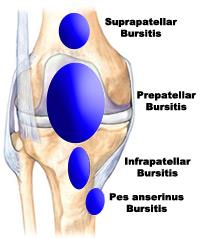
The knee is the largest joint in the body. It is built for weight bearing, stability and mobility. The knee complex is composed of four bones and three osseous bone-to-bone joints. These are the patellafemoral joint, tibiofemoral joint and the tibiofibular joint. The knee joint is surrounded by eleven bursae. A bursa is a fluid filled sack that serves to reduce friction between tendons, and between tendons and bone. The four major bursae of the knee are:
- Suprapatella bursa is located between the distal femur (leg bone) and the quadriceps tendon. It permits free movement of the quadriceps tendon over the distal femur. It allows for full flexion (bending) and extension (straightening) of the knee. It can be irritated by a direct blow or from repeated stress or motions.
- Prepatella bursa is located at the top of the knee over the kneecap. Bursitis of the prepatella bursa is sometimes called carpet layer’s knee, housemaid’s knee or roofer’s knee. It can be caused by a direct blow to the knee or from being in a prolonged kneeling position.
- Infrapatella Bursa is located below the kneecap, under the large patella tendon. It is commonly associated with patella tendonitis or from a repetitive jumping injury called “jumper’s knee.”
- Anserine Bursa is located on the medial or inside of the knee. It is in the area where the hamstring muscle attaches to the lower leg. When inflamed this bursa can produce pain in the inside of the knee when descending stairs.
What is a Bursa?
A bursa is a thin sack filled with synovial fluid, the body's own natural lubricating fluid. This slippery sack allows different tissues such as muscle, tendon, and skin slide over bony surfaces without catching. Your bursa essentially reduces the friction between structures.
A bursa is normally very thin, but they can become inflamed and irritated. This is what is known as bursitis.
What Causes Knee Bursitis?
There is a myriad of factors that can contribute to knee bursitis. The most common ones include:
- Direct trauma or blow to the knee.
- Frequent falls on the knee.
- Repeated pressure on the knee (eg from activities that entail prolonged periods of kneeling) or repetitive minor trauma to the knee.
- Knee Arthritis, thus bursitis can be associated with such conditions as gout, rheumatoid arthritis, and osteoarthritis.
What are the Symptoms of Knee Bursitis?
The symptoms of knee bursitis include:
- Swelling over, above or below the kneecap.
- Limited motion of the knee.
- Redness and warmth at the site of the bursa.
- Painful movement of the knee.
Knee bursitis swelling is within the bursa, not the knee joint. People often call any swelling of the knee joint "water on the knee," but there is an important difference between fluid accumulation within the bursa and within the knee joint.
Symptoms of knee bursitis are usually aggravated by kneeling, crouching, repetitive bending or squatting and symptoms can be relieved when sitting still.
How is Knee Bursitis Diagnosed?
Your physiotherapist will provide you with a thorough quiz of your medical history and a physical examination of your knee to determine if you have knee bursitis. If there is localised swelling and you feel tenderness over the bursa when pressure is applied, a diagnosis is confirmed.
With respect to scans, an MRI or Ultrasound are the most effective for a definitive diagnosis of knee bursitis.
Prognosis
In general, patients respond well to conservative treatment of knee bursitis. It is important that once the pain and inflammation is reduced and motion and strength are restored that the patient gradually returns back to full activities. Instruction in daily activities or sport performance is helpful to reduce the chance of a reoccurrence of the bursitis. In most cases full return to activity will take from 2-6 weeks depending on the severity of the condition. As a preventive measure individuals should:
- Make modifications in work or daily activities such and kneeling, squatting or wearing protective equipment to avoid prolonged pressure or unexpected blows on the bursa.
- Maintain strength and flexibility to reduce stress on the bursa and tendons of the knee.
- Avoid highly repetitive activities whenever possible.
What is the Treatment of Knee Bursitis?
The diagnosis is the easy part. Your physiotherapist will also undertake a biomechanical analysis to determine what the cause of your bursitis actually is. Factors may include muscle weakness, tightness, pain inhibition, leg length discrepancy, training techniques and more.
Physiotherapy
Many patients with knee bursitis start to feel better within a few weeks of the injury. Physiotherapy treatment will aim to:
- Reduce pain and inflammation, this is achieved with the application of electrical modalities, ice, therapeutic taping and education regarding activity modification
- Normalise your knee joint range of motion.
- Strengthen your knee muscles: quadriceps and hamstrings.
- Strengthen your lower limb: calves, hip and pelvis muscles.
- Normalise your muscle lengths.
- Improve your proprioception, agility and balance.
- Improve your technique and function eg walking, running, squatting, hopping and landing.
- Minimise your chance of re-aggravation.
Anti-inflammatories or NSAIDs are also used in combination with physiotherapy to help alleviate the pain and swelling. If the bursa becomes infected or if your symptoms persist for a prolonged period your doctor may recommend that the bursa is aspirated. Alternatively, your doctor may also recommend an injection of a glucocorticoid steroid that is mixed with a local anaesthetic. If infection occurs, you may require antibiotics.
Physical Therapy Management
The treatment of a bursitis is
comparable with the treatment of an overuse injury. (Level of evidence 2a). The therapist will often begin with
soft tissue massages, this is important for the throphycity and better
vascularity. This is followed by some mobilisations in flexion; it is the only
anatomic position where a movement restriction can occur. This is possible
because of the swelling. When the passive mobilisations are done the
physiotherapist will give some light exercises to the patient. A nice example
of such an exercise is when the patient sits on the edge of the table and
lightly lifts and then drops the knee again. As soon as the patient can fulfil
the exercises without any pain, the physiotherapist will step on to more
specific exercises based on muscle-strengthening en flexibility.
An important exercise is the static contraction of the quadriceps (Level of
evidence 5). This should be an exercise that the patient can fulfill at home 1
to 3 times a day.
The objective of the rehabilitation is that patient can resume their everyday activities. The patient must push a towel into the table by using his quadriceps. To see if the exercise is working you have to put your fingers on the inner side of the quadriceps, you will feel the muscle tighten during the contraction of the muscle. The patient has to hold his contraction during 5 seconds; the exercise can be repeated 10 times as hard as possible. It is important not to forget this exercise must be pain free.
Also the stretching of the quadriceps is a good exercise for the patient, it reduces the friction between the skin and the patella tendon. There is less friction when the patella tendon is more flexible. The physiotherapist can also help the patient by using electrotherapy, schooling and giving advice. This advice shall mostly be about how to make the right movements. Ultrasound on the prepatellar bursitis is a treatment that’s not often used.
Besides the Rest, Ice, Compression and Elevation (=RICE) –method (Level of evidence 2a) is a common used treatment for prepatellar bursitis. The ‘rest-phase’ consists a short period of immobilization. This period should be limited to the first days after the trauma. Resting will reduce the metabolic demands of the injured tissue and will avoid increased blood flow.
The use of ice will cause a decrease of the temperature of the tissues in question, inducing vasoconstriction and a limitation of the bleeding. Also the pain will decrease because the ice will occur increasing threshold levels in the free nerve endings and at synapses. Don’t put the ice too long on your knee (maximum 20 minutes at a time with an interval of 30-60 minutes). The compression will decrease the intramuscular blood flow to the affected area and will also reduce the swelling. At last there is the elevation. This ensures that the hydrostatic pressure will decrease and it will also reduce the accumulation of interstitial fluid. This part of the Rice-principe also decreases the pressure in local blood vessels and helps to limit the bleeding. However, the effectiveness of this RICE-method has not been proven in any randomized clinical trial.
In some cases there may be an aspiration of the fluid and an infiltration with an anti-inflammatory drug. (Level of evidence 2a).
Common Physical Therapy interventions in the treatment of Knee Bursitis include:
- Manual Therapeutic Technique (MTT): hands on care including soft tissue massage, stretching and joint mobilization by a physical therapist to regain mobility and range of motion of the knee. Use of mobilization techniques also help to modulate pain.
- Therapeutic Exercises (TE) including stretching and strengthening exercises to regain range of motion and strengthen muscles of the knee to support, stabilize, and decrease the stresses place on the bursa and tendons of the knee joint.
- Neuromuscular Reeducation (NMR) to restore stability, retrain the lower extremity and improve movement techniques and mechanics (for example, running, kneeling, squatting and jumping) of the involved lower extremity to reduce stress on bursa and tendons in daily activities.
- Modalities including the use of ultrasound, electrical stimulation, ice, cold laser and others to decrease pain and inflammation of the involved bursa.
- Home program including strengthening, stretching and stabilization exercises and instructions to help the person perform daily tasks and advance to the next functional level.
Knee Bursa Surgery?
In particularly stubborn cases, surgical removal of the bursa may be recommended.
Risks of surgery include infection, persistent instability and pain, stiffness, and difficulty returning to your previous level of activity. The good news is that more than 90% of patients have no complications post-surgery.
Post-Surgical Rehabilitation
Post-operative knee rehabilitation is one of the most important, yet too often neglected, aspects of knee surgery. The most successful and quickest outcomes result from the guidance and supervision of an experienced physiotherapist.
How Can You Prevent Knee Bursitis?
Knee bursitis is best prevented by maintaining flexible thigh muscles and reducing the amount of time you are in a kneeling position. Ice after excessive kneeling is recommended to avoid an inflammatory response, which is the first stage of bursitis.
Pacing yourself during activities which entail repeated bending or squatting is also paramount. Ensuring that you take regular rest breaks between periods of bending or kneeling and alternating them with other less aggravating activities is key. Essentially, an appropriate balance between rest and activity is recommended. Weight-management can play a role in the pressure exerted on lower limb joints, and thus should be something considered as a long-term preventative measure.
For more advice, please consult your physiotherapist.