Patellofemoral Pain Syndrome and Rehabilitation Exercises
What Is Patellofemoral Pain Syndrome? (Aka Runner’s knee)
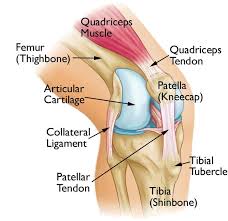
Patellofemoral pain syndrome (PFPS), also known as runner’s knee, is the most common of all kinds of knee pain, causing pain around and under the kneecap. Almost anyone can get it, but it particularly affects runners, cyclists and hikers, and also office workers or anyone else who sits for a living. PFPS is an umbrella term used for pain arising from the patellofemoral joint itself, or adjacent soft tissues. Historically it has been referred to as anterior knee pain but this is misleading as the pain can be felt in all aspects of the knee (including the popliteal fossa).
The kneecap (patella) moves up and down, tilts, and rotates. Patellofemoral pain syndrome is pain under and around the kneecap from changes in the patellofemoral joint. One or both knees can have it. High-impact sports such as football, basketball, soccer, tennis, and running can worsen kneecap problems. Running on uneven surfaces (hills or trails) or playing on different surfaces (grass and hard tennis courts) may also lead to this syndrome. Even sitting for long periods can hurt (moviegoer’s knee).
What Causes Patellofemoral Pain Syndrome?
The causes include weak quadriceps muscles (front of the thigh), tight hamstrings (back of the thigh) or calf muscles, and weak or tight hip muscles. It’s an overuse syndrome and can affect active people such as runners. It’s also an overload syndrome because it affects inactive people (who are overweight).
What Are the Symptoms of Patellofemoral Pain Syndrome?
Dull, aching kneecap pain occurs with activity and often worsens when going down steps or hills or when sitting. The knee can catch when bending. A painful grating or creaking feeling can occur.
How Is Patellofemoral Pain Syndrome Diagnosed?
The health care provider will make a diagnosis from the medical history and physical examination. X-rays of the knees, magnetic resonance imaging (MRI), and arthroscopy may be done when diagnosis is unclear. In arthroscopy, the health care provider puts a tiny camera into the knee to see inside.
How Is Patellofemoral Pain Syndrome Treated?
First treatment is rest, quadriceps strengthening exercises, and icing (especially after exercise, used for 10 to 20 minutes). If possible, change to non-impact aerobic activities, such as swimming or elliptical exercise machines. Hip, hamstring, calf, and iliotibial band stretching exercises may also help. It’s important to wear the right footwear, such as running shoes with extra cushioning and arch supports. Most runners, for example, change shoes every 300 to 500 miles. Orthotics, knee sleeves, and braces may be of benefit. Surgery is the last resort. Recovery can take up to 6 weeks.
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, help inflammation (swelling, redness) and pain. These drugs can cause stomach problems and should be taken with meals. People who have ulcers or bleeding ulcers should not use these drugs or check with the health care provider.
Kneecap pain can often be managed with physical therapy to strengthen quadriceps muscles and stretch hamstring and calf muscles.
DO’s in Managing Patellofemoral Pain Syndrome:
- DO take your medicines as prescribed.
- DO call your healthcare provider if you have side effects from medicines.
- DO stop the activity that causes pain.
- Choose a low impact exercise.
- Incorporate a warm up before exercise and a warm down after exercise.
- Reduce weight if you’re overweight.
- Maintain a healthy weight.
- Restart the activity that caused the pain very carefully.
- DO continue for life the exercises to strengthen knee, hamstring, and calf muscles that you learn in physical therapy.
- DO call your Physical Therapist or health care provider if you tried conservative treatment on your own and still have symptoms.
DON’Ts in Managing Patellofemoral Pain Syndrome:
- DON’T self-medicate before you see your healthcare provider.
- DON’T use NSAIDs if you had bleeding ulcers.
- DON’T do bent knee exercises, such as squats, deep knee bends, or 90-degree leg extensions until you’re cleared from your Physiotherapist.
- DON’T continue the offending activity, such as running until you’re cleared from your Physiotherapist. You can worsen the injury or damage the joint itself.
Treatment
The management of PFPS should focus on the implementation of a comprehensive rehabilitation program. It is important to communicate to the patient that a successful return to recreational or competitive activities requires compliance with the rehabilitation plan.
RELATIVE REST
Reduction of loading to the patellofemoral joint and surrounding soft tissues is the first step to reduce pain. If resistance training exercises have been identified as playing a role in causing the injury, cessation of specific exercises such as full squats and lunges is indicated.
Runners should reduce mileage to a level that does not provoke pain (while running or the day after running). Alternative activities such as bicycling, swimming, or the use of an elliptical trainer can be used to maintain fitness while treatment is ongoing. Ice or other methods of cold application may further reduce symptoms.
ADDRESSING THE UNDERLYING CAUSE
In most patients with PFPS, a careful history will identify a precipitating event. Changes in activity patterns, such as an increase in running mileage, running stadium steps for conditioning, or the addition of resistance training exercises that affect the patellofemoral joint, often are associated with symptom onset. Excessively worn or inappropriate footwear also may contribute. Discussing these issues with the patient and developing a specific plan to avoid repeating the causal behavior are important in preventing a recurrence.
PHYSICAL THERAPY
A well-structured rehabilitation program is the mainstay of treatment. Several studies have shown physical therapy to be effective in treating PFPS. However, there is no one program that will be effective for all patients. The rehabilitation program should focus on correcting mal-tracking of the patella by addressing the findings identified on the physical examination.
Some patients may require significant strengthening of the quadriceps. Others may have excellent quadriceps strength but excessively tight lateral structures or poor quadriceps flexibility. Soft tissue techniques and flexibility exercises can be helpful for these patients. A detailed assessment of the imbalances of patellar tracking is therefore essential to tailoring treatment. Specific exercises can then be prescribed as part of a home rehabilitation program. Patients who require further assessment or ongoing instruction can be referred to a physical therapist.
OTHER TREATMENTS
- Analgesics. Although nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed for patients with PFPS, there is little evidence supporting their effectiveness. NSAIDs or acetaminophen may be considered at the initiation of treatment for patients with symptoms during daily activities and for those whose symptoms are not controlled with ice applications.
- Bracing. A variety of braces, sleeves, and straps have been used in the treatment of PFPS. Although bracing alone may provide some symptomatic relief, depending on the cause of the PFPS.
- Patellar Taping. Patellar taping has been suggested as a method to treat PFPS by improving alignment and quadriceps function. Although the results from uncontrolled studies were encouraging, the results of three randomized clinical trials have not been consistent: two found no benefit when patellar taping was added to a program of physical therapy. More studies are needed to determine the role of patellar taping in treating PFPS.
- Foot Orthoses. As discussed above, prospective studies have yet to demonstrate strong relationships between static measures of lower extremity malalignment and lower extremity injuries. Moreover, alignment was not found to be predictive of outcome in patients with PFPS in two long-term studies. Other studies, however, have shown that orthoses can be effective in some patients with PFPS. Over-the-counter soft orthoses are a reasonable choice for patients who have PFPS with malalignment. For those with persistent symptoms, a custom orthotic can be considered.
Rehabilitation Exercises for Patellofemoral Pain Syndrome (Runner’s Knee)
You can do the hamstring stretch right away. When the pain in your knee has decreased, you can do the quadriceps stretch and start strengthening the thigh muscles using the rest of the exercises.
Standing Hamstring Stretch
Place the heel of
your injured leg on a stool about 15 inches high. Keep your knee straight. Lean
forward, bending at the hips until you feel a mild stretch in the back of your
thigh.  Make sure you do not roll your shoulders and bend at the waist when
doing this or you will stretch your lower back instead of your leg. Hold the
stretch for 15 to 30 seconds. Repeat 3 times.
Make sure you do not roll your shoulders and bend at the waist when
doing this or you will stretch your lower back instead of your leg. Hold the
stretch for 15 to 30 seconds. Repeat 3 times.
Quadriceps stretch
 Stand an arm’s length
away from the wall with your injured leg farthest from the wall. Facing
straight ahead, brace yourself by keeping one hand against the wall. With your
other hand, grasp the ankle of your injured leg and pull your heel toward your
buttocks. Don’t arch or twist your back. Keep your knees together. Hold this
stretch for 15 to 30 seconds.
Stand an arm’s length
away from the wall with your injured leg farthest from the wall. Facing
straight ahead, brace yourself by keeping one hand against the wall. With your
other hand, grasp the ankle of your injured leg and pull your heel toward your
buttocks. Don’t arch or twist your back. Keep your knees together. Hold this
stretch for 15 to 30 seconds.
Side-lying leg lift
 Lying on your
uninjured side, tighten the front thigh muscles on your top leg and lift that
leg 8 to 10 inches away from the other leg. Keep the leg straight and lower
slowly. Do 3 sets of 10.
Lying on your
uninjured side, tighten the front thigh muscles on your top leg and lift that
leg 8 to 10 inches away from the other leg. Keep the leg straight and lower
slowly. Do 3 sets of 10.
Quad sets
Sitting on the floor
with your injured leg straight and your other leg bent, press the back of the
knee of your injured leg against the floor by tightening the muscles on the top
of your thigh.  Hold this position 10 seconds. Relax. Do 3 sets of 10.
Hold this position 10 seconds. Relax. Do 3 sets of 10.
Straight leg raise
 Lie on your back with
your legs straight out in front of you. Bend the knee on your uninjured side
and place the foot flat on the floor. Tighten the thigh muscle of the other leg
and lift it about 8 inches off the floor, keeping the thigh muscle tight
throughout. Slowly lower your leg back down to the floor. Do 3 sets of 10.
Lie on your back with
your legs straight out in front of you. Bend the knee on your uninjured side
and place the foot flat on the floor. Tighten the thigh muscle of the other leg
and lift it about 8 inches off the floor, keeping the thigh muscle tight
throughout. Slowly lower your leg back down to the floor. Do 3 sets of 10.
Step-up
 Stand with the foot
of your injured leg on a support (like a small step or block of wood) 3 to 5
inches high. Keep your other foot flat on the floor. Shift your weight onto
your injured leg on the support straighten your knee as the other leg comes off
the floor. Lower your leg back to the floor slowly. Do 3 sets of 10.
Stand with the foot
of your injured leg on a support (like a small step or block of wood) 3 to 5
inches high. Keep your other foot flat on the floor. Shift your weight onto
your injured leg on the support straighten your knee as the other leg comes off
the floor. Lower your leg back to the floor slowly. Do 3 sets of 10.
Wall squat with a ball
 Stand with your back,
shoulders, and head against a wall and look straight ahead. Keep your shoulders
relaxed and your feet 2 feet away from the wall and a shoulder’s width apart.
Place a soccer or basketball-sized ball behind your back. Keeping your back upright,
slowly squat down to a 45-degree angle. Your thighs will not yet be parallel to
the floor. Hold this position for 10 seconds and then slowly slide back up the
wall. Repeat 10 times. Build up to 3 sets of 10.
Stand with your back,
shoulders, and head against a wall and look straight ahead. Keep your shoulders
relaxed and your feet 2 feet away from the wall and a shoulder’s width apart.
Place a soccer or basketball-sized ball behind your back. Keeping your back upright,
slowly squat down to a 45-degree angle. Your thighs will not yet be parallel to
the floor. Hold this position for 10 seconds and then slowly slide back up the
wall. Repeat 10 times. Build up to 3 sets of 10.
Knee stabilization
Wrap a piece of elastic tubing around the ankle of the uninjured leg. Tie a knot in the other end of the tubing and close it in a door.
 1. Stand facing the
door on the leg without tubing and bend your knee slightly, keeping your thigh
muscles tight. While maintaining this position, move the leg with the tubing
straight back behind you. Do 3 sets of 10.
1. Stand facing the
door on the leg without tubing and bend your knee slightly, keeping your thigh
muscles tight. While maintaining this position, move the leg with the tubing
straight back behind you. Do 3 sets of 10.
2. Turn 90 degrees so the leg without tubing is closest to the door. Move the leg with tubing away from your body. Do 3 sets of 10.
3. Turn 90 degrees again so your back is to the door. Move the leg with tubing straight out in front of you. Do 3 sets of 10.
4. Turn your body 90 degrees again so the leg with tubing is closest to the door. Move the leg with tubing across your body. Do 3 sets of 10.
Hold onto a chair if you need help balancing. This exercise can be made even more challenging by standing on a pillow while you move the leg with tubing.
Resisted terminal knee extension
 Make a loop with a
piece of elastic tubing by tying a knot in both ends. Close the knot in a door
at knee height. Step into the loop with your injured leg so the tubing is
around the back of your knee. Lift the other foot off the ground and hold onto
a chair for balance, if needed. Bend the knee with tubing about 45 degrees.
Slowly straighten your leg, keeping your thigh muscle tight as you do this.
Repeat 15 times. Do 2 sets of 15. If you need an easier way to do this, stand
on both legs for better support while you do the exercise.
Make a loop with a
piece of elastic tubing by tying a knot in both ends. Close the knot in a door
at knee height. Step into the loop with your injured leg so the tubing is
around the back of your knee. Lift the other foot off the ground and hold onto
a chair for balance, if needed. Bend the knee with tubing about 45 degrees.
Slowly straighten your leg, keeping your thigh muscle tight as you do this.
Repeat 15 times. Do 2 sets of 15. If you need an easier way to do this, stand
on both legs for better support while you do the exercise.
Standing calf stretch
 Facing a wall, put
your hands against the wall at about eye level. Keep one leg back with the heel
on the floor, and the other leg forward. Turn your back foot slightly inward
(as if you were pigeon-toed) as you slowly lean into the wall until you feel a
stretch in the back of your calf. Hold for 15 to 30 seconds. Repeat 3 times and
then switch the position of your legs and repeat the exercise 3 times. Do this
exercise several times each day.
Facing a wall, put
your hands against the wall at about eye level. Keep one leg back with the heel
on the floor, and the other leg forward. Turn your back foot slightly inward
(as if you were pigeon-toed) as you slowly lean into the wall until you feel a
stretch in the back of your calf. Hold for 15 to 30 seconds. Repeat 3 times and
then switch the position of your legs and repeat the exercise 3 times. Do this
exercise several times each day.
Clam exercise
 Lie on your uninjured
side with your hips and knees bent and feet together. Slowly raise your top leg
toward the ceiling while keeping your heels touching each other. Hold for 2
seconds and lower slowly. Do 3 sets of 10 repetitions.
Lie on your uninjured
side with your hips and knees bent and feet together. Slowly raise your top leg
toward the ceiling while keeping your heels touching each other. Hold for 2
seconds and lower slowly. Do 3 sets of 10 repetitions.
Iliotibial band stretch: Side-bending
Cross one leg in front of the other leg and lean in the opposite direction from the front leg. Reach the arm on the side of the back leg over your head while you do this. Hold this position for 15 to 30 seconds. Return to the starting position. Repeat 3 times and then switch legs and repeat the exercise.