Physiotherapy Management of Urinary Incontinence in Females
Introduction
Urinary incontinence (UI) is a prevalent and bothersome condition affecting women of all ages. UI can be treated with lifestyle interventions, bladder training, electrical stimulation, surgery and pelvic floor muscle training (PFMT) with or without biofeedback.
There is some evidence that lifestyle interventions (such as weight reduction in obese women) and bladder training may have some effect in reducing UI. The evidence for electrical stimulation is debated. Surgery carries a risk of complications and the long-term outcome is questionable. This leaves PFMT as the main physiotherapy intervention for UI. The NICE guideline states that PFMT is just as effective as surgery for around half of women with stress urinary incontinence. There is Level 1 evidence (recommendation A) that PFMT should be first-line treatment for UI in females. This review summarises: the burden of UI for individuals and the healthcare system; background information about how PFMT can prevent and treat UI; the evidence about the effects of PFMT on female UI, with a special focus of the effect of group PFMT; and future directions for research and practice.
Urinary incontinence is the involuntary leakage of urine. It means a person urinates when they do not want to. Control over the urinary sphincter is either lost or weakened. Urinary incontinence is a common problem that affects many people. According to the American Urological Association, one-quarter to one-third of men and women in the United States experience urinary incontinence.
Urinary incontinence is more common among women than men. An estimated 30 percent of females aged 30-60 are thought to suffer from it, compared to 1.5-5 percent of men.
Identifying the classification of urinary incontinence can help to guide treatment, however, an individual could exhibit symptoms from more than one of the classifications.
Classifications of Urinary Incontinence
- Stress Urinary Incontinence: Complaint of involuntary loss of urine on effort or physical exertion (e.g. sporting activities), or on sneezing or coughing.
- Urgency Urinary Incontinence: Complaint of involuntary loss of urine associated with urgency.
- Mixed Urinary Incontinence: Complaint of involuntary loss of urine associated with urgency and also effort or physical exertion or on sneezing or coughing.
- Overactive Bladder (OAB, Urgency) Syndrome: Urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology.
Urgency: Complaint of a sudden, compelling desire to pass urine which is difficult to defer.
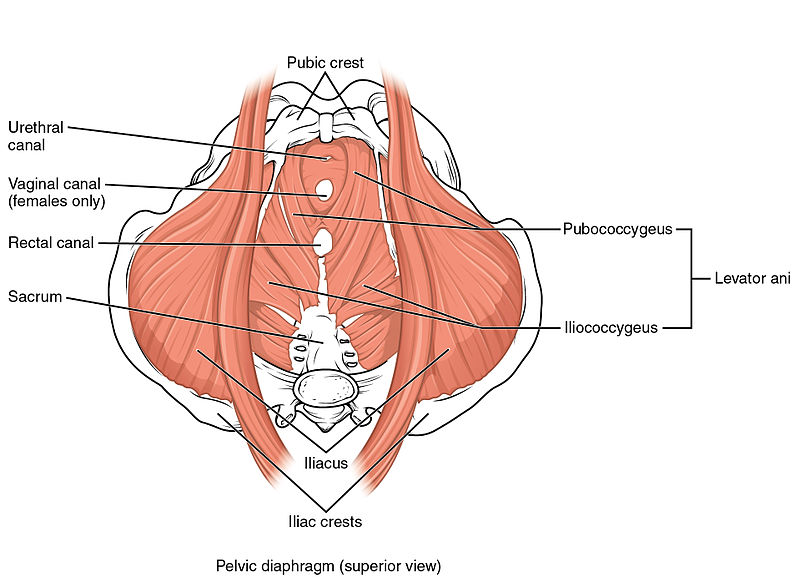
Clinically Relevant Anatomy of Pelvic Floor
The pelvic floor is made up of the muscles, ligaments, and fascial structures that act together to support the pelvic organs and to provide compressive forces to the urethra during increased intra-abdominal pressure. The pelvic floor muscles refer to the muscular layer of the pelvic floor. It includes the levator ani, striated urogenital sphincter, external anal sphincter, ischiocavernosus, and bulbospongiosus.
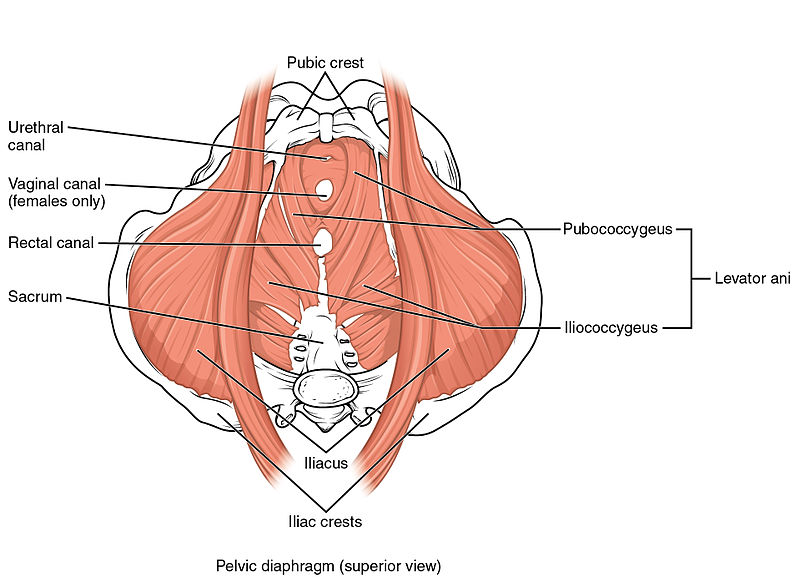
The urethra, vagina, and rectum pass through the pelvic floor and are surrounded by the pelvic floor muscles. During increased intra-abdominal pressure, the pelvic floor muscles must contract to provide support. When the pelvic floor muscles contract the urethra, anus, and vagina close. The contraction is important in preventing involuntary loss of urine or rectal contents. The pelvic floor muscles must also relax in order to void.
The Female Pelvic Floor
The female pelvic floor consists of fascias, ligaments and the pelvic floor muscles (PFM). The PFM form the base of the abdominal cavity on which the pelvic organs rest, and where the urethra, vagina and rectum pass through. The area surrounding the three openings of the pelvic floor in women is named levator hiatus and is the largest hernia port in the body. In pelvic organ prolapse either the bladder, uterus or rectum, or all these organs protrude through the vagina. The PFM comprise three layers of muscles, with the different muscles having different origins, insertions and fibre directions (Figure 1).
Figure 1. Anatomy of the pelvic floor muscles in women. A. Superior view of the pelvic floor in the transverse plane, with pubic symphysis at the bottom. B. Inferior view of the pelvic floor in the transverse plane, with pubic symphysis at the top.
There is continuous muscle activity of the PFM, except just before and during voiding and defaecation. If each muscle of the pelvic floor was able to contract separately, each muscle would have a different function. However, a voluntary contraction of the PFM implies a mass contraction observed as a squeeze around the openings and a lift of the pelvic floor in a forward and inward (cranial) direction.
In an intact and well-functioning pelvic floor, the connective tissue of the ligaments and fascias and the PFM act together to counteract the impact of any increase in intra-abdominal pressure and ground reaction forces, keeping the pelvic organs in place with little downward movements and little or no opening of the levator hiatus area or the urethra. This is an automatic function, and for women with a well-functioning pelvic floor and no symptoms there is no need to think about voluntarily contracting the PFM. If, for some reason, this entity is not working adequately (e.g. due to inherited morphological factors or acquired factors) pelvic floor dysfunctions may occur. Pelvic floor dysfunctions include UI, anal incontinence, pelvic organ prolapse, sensory and emptying abnormalities of the lower urinary tract, defecatory dysfunction, sexual dysfunction and chronic pain syndromes.
Bump and Norton developed a model describing possible aetiological factors in pelvic floor dysfunctions in women. Each factor is classified as predisposing, inciting, promoting or decompensating, as shown in Box 1. DeLancey et al further developed this model into an integrated lifespan model, where they used a graphical tool to integrate pelvic floor function related to pelvic floor disorders in three major phases. These phases are: development of functional reserve during an individual’s growth; variations in the amount of injury and potential recovery that occur during and after vaginal birth; and deterioration occurring with advancing age.
Box 1
Categories of Aetiological Factors in Pelvic Floor Dysfunctions.
|
Predisposing Gender Genetic Neurological Anatomical Collagen Muscular Cultural Environmental |
Inciting Childbirth Nerve damage Muscle damage Radiation Tissue disruption Radical surgery |
Promoting Constipation Occupation Recreation Obesity Surgery Lung disease Smoking Menstrual cycle Infection Medication Menopause |
Decompensating Ageing Dementia Debility Disease Environment Medications |
Established risk factors for UI are age, body mass index, parity and mode of delivery, with vaginal birth being the most significant. However, the prevalence of UI is high among women who exercise, and young, nulliparous, female elite athletes. The prevalence is generally higher in women performing sports involving high-impact activities (jumping and running), but there is still little knowledge on women participating in weightlifting and strength-demanding sports. A prevalence as high as 80% has been found in trampoline jumpers. As SUI occurs during physical exertion/activity, the activity level of the studied population is an important factor to consider when comparing the results of prevalence studies and risk factors. Female athletes are about three times more likely to experience UI compared with controls.
The Pelvic Floor Muscles and Mechanism of Action in Urgency
and Stress Urinary Incontinence
The PFM are the only muscles in the body with an anatomical location surrounding the levator hiatus and the three pelvic openings in women. Bo et al described a possible mechanism for how voluntary contraction of the PFM and strength training over time may positively affect PFM function and prevent and treat UI.
A single voluntary contraction of the PFM increases urethral closure pressure, causes simultaneous co-contraction of the urethral sphincter and reduces the levator hiatus area by 25% from a resting area of 20 cm2 (95% CI 17 to 23) to 15 cm2 (95% CI 13 to 17). The muscle length shortens 21% from 12.5 cm (95% CI 11.1 to 13.8) to 9.7 cm (95% CI 8.7 to 10.7), and lifts the pelvic floor higher up in the pelvis, stabilising the pelvic floor. One approach, known as ‘the Knack’, is to practice pre/co-contraction of the PFM during situations where such contractions are needed to prevent loss of urine. However, it is unknown whether this approach leads to automatic pre/co-contraction of the PFM during such situations.
An assessor-blinded randomized controlled trial involving 109 women with pelvic organ prolapse and comorbidities such as UI and anal incontinence found that 6 months of PFMT caused permanent morphological improvements of the pelvic floor. These morphological changes included elevation of the bladder neck and rectal ampulla by approximately 0.5 cm, narrowing of the hiatal area by 6%, greater muscle thickness by 16% and reduced muscle length by 4%. In that trial, there was less opening of the hiatal area and less increase in muscle length during straining in the PFMT group, which may indicate automatic function and increased PFM stiffness. Moreover, several randomized trials have found that women who have trained the PFM have significantly less incontinence during running and jumping (without voluntary contraction) than controls, indicating a positive effect on automatic function. Hence, there are rationales related to anatomy, biomechanics and exercise physiology that support PFMT in the treatment of UI and pelvic organ prolapse.
As the cause of UUI in non-neurogenic patients is unknown, the rationale for PFMT in the group of patients with overactive bladder is not as clear as for SUI. However, a voluntary contraction of the PFM has been shown to inhibit the urge to void, detrusor contraction and urinary leakage. To date there is no knowledge about how strong this voluntary contraction needs to be to influence urethral closure pressure. It is also unknown whether PFMT over time is needed in addition to the immediate effect of the voluntary contraction during urge to void to treat UUI and other symptoms of overactive bladder.
Effect of Pelvic Floor Muscle Training on Urinary Incontinence in Females Treatment
There is Level 1 evidence (recommendation A) that PFMT should be first-line treatment for UI in females. In the general population, women with SUI who perform PFMT are 8 times (95% CI 4 to 19; 56% versus 6%) more likely to be cured than control groups with no or sham treatments. PFMT reduced UI episodes among women with SUI (MD 1.2 episodes per day, 95% CI 0.7 to 1.8) and among women with any type of UI (MD 1.0 episode per day, 95% CI 0.6 to 1.4). On short pad tests, PFMT reduced the amount of urine lost by women with SUI (MD 10 g, 95% CI 1 to 19) and by women with any type of UI (MD 4 g, 95% CI 2 to 5). PFMT also caused women with any type of UI to report significantly better incontinence-related quality of life and reduced UI symptoms than those who did not receive the treatment. Because of substantial heterogeneity among the outcome measures used to assess quality of life, meta-analyses were not conducted. PFMT has rare and minor adverse effects.
The effects of PFMT are better if it is delivered with regular supervised training (e.g. once a week). Supervised training is defined as a PFMT program taught and monitored by a health professional/clinician/instructor. This means that the Physiotherapist cues each PFM contraction either individually or in a group setting. If the physiotherapist only provides teaching and assessment at the first consultation, this is not considered to be supervised training.
To date, the Cochrane reviews have not distinguished between different subgroups of UI but have concluded that PFMT is consistently more effective in women with SUI only than in women with mixed urinary incontinence or UUI. A recent systematic review of the effects of PFMT in women with only overactive bladder symptoms (including UUI) included 11 randomized trials. The heterogeneity of outcome measures and intervention protocols was substantial, so a meta-analysis of the included studies was not conducted. Approximately half of the studies showed a positive effect of PFMT and half of them did not. Most of the study protocols included regular strength training of the PFM that was similar to PFMT protocols for SUI, while three of the protocols also included training of a voluntary contraction to inhibit urge to void and detrusor contraction.
Prevention
In randomized trials involving women with and without UI during pregnancy, PFMT produced a 26% reduced risk (RR 0.74, 95% CI 0.61 to 0.90) of UI during pregnancy and the mid-postnatal period (RR 0.73, 95% CI 0.55 to 0.97). Moreover, pregnant continent women who exercise the PFM during pregnancy (primary prevention) are 62% less likely (RR for incontinence 0.38, 95% CI 0.20 to 0.72) to experience UI in late pregnancy and have 29% lower risk (RR 0.71, 95% CI 0.54 to 0.95) of UI 3 to 6 months after giving birth.
To date there is insufficient evidence for a long-term effect of antenatal PFMT beyond 6 to 12 months postpartum. However, long-term studies of any healthcare intervention are generally difficult to conduct due to loss to follow-up, the ethical demand to offer the control group the active intervention in a reasonable timeframe, co-interventions, and competing and recurrent events in the follow-up period. This is especially challenging in the peripartum period because many women become pregnant again during the follow-up period.
As for any exercise intervention, it is expected that the benefits gained from PFMT need maintenance training for continuing effects. A systematic review on the long-term effects of PFMT included 19 studies with follow-up periods of 1 to 15 years; long-term adherence to PFMT varied between 10 and 70%. Among participants who were treated with PFMT and whose UI resolved initially, five studies reported sustained success rates (ie, percentage remaining free of UI at long-term follow-up), which were between 41 and 85%. Surgery rates in the long term varied between 5 and 58%. It was concluded that the short-term benefit of PFMT can be maintained at long-term follow-up without incentives for continued training, although there was high heterogeneity in both interventional and methodological quality in short-term and long-term PFMT studies.
Group Pelvic Floor Muscle Training
The first randomized controlled trial assessing the effect of group training of the PFM came from Norway in 1990. Only women with urodynamically proven SUI were included in the study. All women received the same teaching about how to perform a correct PFM contraction, and ability to contract was assessed by visual observation and vaginal palpation. Vaginal resting pressure, PFM strength (maximal voluntary contraction) and endurance were measured by a vaginal manometer (high-precision microtip pressure transducer connected to a vaginal balloon) before randomisation.
For the PFMT protocols, both groups were asked to perform three sets of eight to twelve contractions per day at home and had follow-up appointments once a month for 6 months with a trained physiotherapist for measurement of PFM variables. All participants reported training adherence in a diary. In addition to this protocol, the ‘intensive training group’ attended a 1-hour group PFM exercise class once a week. It is worthwhile noting that what was named the ‘home training group’ in this study had more individual visits with a physiotherapist than the intervention group in many other studies (ie, seven visits with assessment of PFM variables and motivation for training). The participants who received the additional group training improved their PFM strength from a mean 7 cmH2O (95% CI 4 to 10) to 23 cmH2O (95% CI 18 to 27). This was significantly better that the ‘home training’ participants, who improved from a mean of 8 cmH2O (95% CI 6 to 10) to 15 cmH2O (95% CI 12 to 19). A pad test with standardised bladder volume, including provocative jumping, running and sit-ups, showed that the participants who received the additional group training improved their UI from a mean of 27 g (95% CI 9 to 45) to 7 g (95% CI 1 to 13). This was again significantly better than the ‘home training’ participants, who improved from a mean of 29 g (95% CI 14 to 44) to 22 g (95% CI 9 to 35). The participants who received the additional group training gained further significant benefits: fewer still had urodynamically proven SUI after treatment, and 60% (versus 17% in the ‘home training’ group) reported that they were cured or almost cured (RR 3.53, 95% CI 1.49 to 8.36). Secondary analyses of those with or without successful outcomes after PFMT found that moderate PFM strength before starting the training was one of four important factors for success. Furthermore, PFM strength development during the exercise period and maximal strength after treatment each correlated with the reduction in UI.
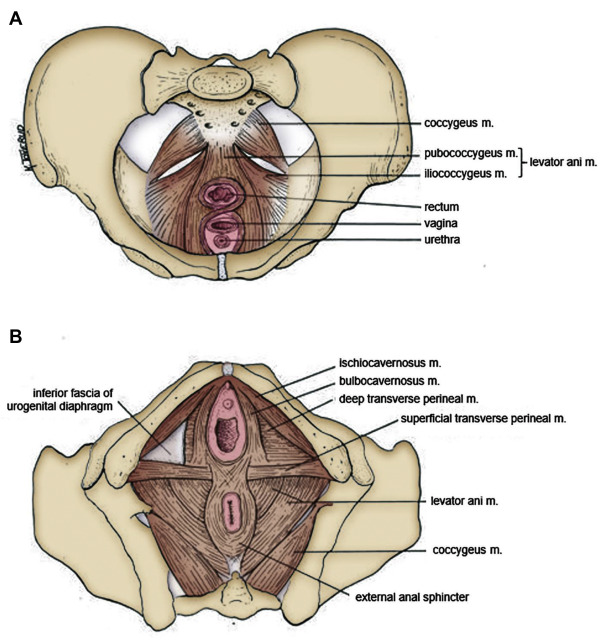
The PFMT protocol used in the successful arm of that trial (ie, weekly group training + daily home exercise) has since been used in several controlled trials in Norway. In a matched controlled trial in postpartum women, Mørkved and Bø found that the training group reduced their prevalence of UI by 50% more than the control group (who received the customary written postpartum instructions), with a benefit maintained at 1-year follow-up. In another trial, 107 women with urodynamically proven SUI were randomised to either the same PFMT group training intervention, electrical stimulation, vaginal weighted cones or usual care. The PFMT group training intervention was superior to electrical stimulation, vaginal weighted cones and the no-treatment control with respect to improvement in PFM strength and reduction in UI on pad test (Figure 2, Figure 3). Mørkved et al and Stafne et al found significantly better results from group PFMT compared with a control group receiving usual care during pregnancy. Statistically significant benefits have also been found in men following the same group training concept.
Surprisingly, one randomised controlled trial that investigated exactly the same exercise protocol did not find any significant benefits over control in a group exercising from 6 to 8 weeks post-partum to 6 months postpartum. However, this trial was specifically aimed at recruiting women with major levator ani defects and the participating women may therefore have not been comparable with women participating in other postpartum studies.
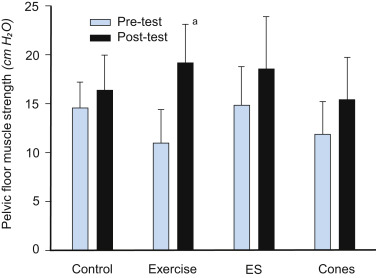
Figure 2. Pelvic floor muscle strength before and after 6 months of either pelvic floor muscle training (exercise), electrical stimulation (ES), use of vaginal cones or no treatment (control). Results are reported as means with 95% CI.
Significant difference in change between control and intervention. Only the exercise group had a statistically significant change in pelvic floor muscle strength compared with the control group.
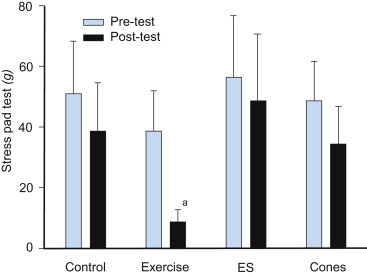
Figure 3. Urinary incontinence measured with a short provocative pad test with standardized bladder volume before and after 6 months of either pelvic floor muscle training (exercise), electrical stimulation (ES), use of vaginal cones or no treatment (control). Results are reported as means with 95% CI.
Statistically
significant difference in change in urinary leakage compared with the control
group.
Group versus Individual Pelvic Floor Muscle Training
A Cochrane review concluded that 90% of those who had combined group and individual supervision reported improvement versus 57% of women receiving individual supervision only (RR for no improvement 0.29, 95% CI 0.15 to 0.55). This meta-analysis was based on only three randomized trials and although the confidence interval was wide, the effect was strong enough to be clearly worthwhile. Since there were differences in health professional contact in those receiving the additional group training and the other PFMT group, it is impossible to separate the effect of the actual additional group training from the extra attention. The Cochrane review found that PFMT was consistently more effective in those receiving more health professional contact. However, attention alone is unlikely to affect UI. In an assessor-blinded randomised trial, Dumoulin et al compared three different interventions: PFMT and electrical stimulation; PFMT, electrical stimulation and transverse abdominal training; and the same attention and time spent with a physiotherapist giving them limb massage. The massage group did not show any improvement in any measures of UI but did improve in disease-specific quality of life.
In a recent systematic review comparing the effect of individual and group PFMT, 10 studies involving group training were included. Five of six randomized trials comparing group PFMT with individual PFMT were included in a meta-analysis. The authors found significant risk of bias in many of the studies: random sequence generation (three of five), allocation concealment (four of five) and blinding of outcome assessment (two of five). The conclusion was that there was no significant difference in results between individual and group-based PFMT. There was high heterogeneity in outcome measures and exercise protocols between studies, but a more serious bias was the difference in supervision and content of the intervention between the individual and group training protocols within the same study.
The only study with a similar dosage of PFMT and attention/supervision by the therapist was the trial by Lamb et al. This study included women with both SUI and UUI. The researchers found no differences in results between group or individual training. However, there were other limitations to this study such as that the duration of the interventions was 3 weeks and there was no assessment of the women’s ability to correctly contract the PFM.
In a well-designed, adequately powered, non-inferiority, multicentre randomized trial involving women with SUI or mixed urinary incontinence, individual PFMT was compared with group training. Both treatment arms contained exactly the same dosage of training and the same contact and attention from the physiotherapist. Furthermore, both groups received the same individual information and underwent assessment and feedback of their ability to contract the PFM before commencing the training period. At 1-year follow-up, the median reduction in the frequency of leakage episodes per week was similar: 70% (95% CI 44 to 89) in the individual group and 74% (95% CI 46 to 86) in the group training group. There were no important between-group differences in any other outcome measures either, and the researchers concluded that group PFMT is not inferior to individual training in treatment of female UI.
Group Training and Ability to Contract the Pelvic Floor Muscles
Several studies have found that > 30% of women with UI are unable to contract the PFM at their first consultation, even after thorough individual instruction. The most common errors are to contract other outer pelvic muscles such as hip adductor, gluteal and abdominal muscles instead of or in addition to the PFM. In addition, Bump et al found that as many as 25% were straining instead of performing a squeeze or inward lift of the pelvic floor. They also found that among women who were able to contract, 49% were performing a contraction of enough intensity to influence the urethral closure pressure.
To be effective in treatment of UI, it is essential that the women can perform a correct contraction and with adequate strength. Most group training regimens of PFMT include individual teaching of a correct contraction and assessment and feedback of ability to contract. However, in a few studies, group training has been performed without such confirmation of the participants’ skills. All these studies found significant improvement in UI after the intervention and no difference between individual or group training.
In a primary prevention study, 169 first-time pregnant women were randomized to either an exercise group including PFMT three times a week or a control group without any intervention. The participants had no evaluation of their ability to perform a correct contraction. The results showed significant differences in incidence, frequency and amount of UI in favour of the exercise group, accompanied by a benefit on an incontinence-related quality of life score with an effect size of 0.8. The results were presented as per protocol analyses only, but show that it is possible to perform effective PFMT without individual teaching and control of ability to perform a correct contraction in a group of women with no symptoms and injuries to the PFM. However, it is unknown whether the effect would have been even higher with additional individual teaching and control of the women’s ability to perform a correct contraction.
Performing a correct PFM contraction can be a special challenge after childbirth. Vermandel et al studied 958 women (mean age 30 years, SD 5) within 1 week postpartum. They asked about experience and knowledge of PFMT using a questionnaire and assessed ability to perform a correct PFM contraction by visual observation of the perineum during contraction attempts. Within the study cohort, 26% had no knowledge of the pelvic floor, 52% had trained the PFM, 52% were unable to contract their PFM, 29% showed no movement at all and 24% showed some movement but no inward displacement. Among those who had trained the PFM and were convinced they were able to contract their PFM correctly, 45% were not. However, after verbal instructions by a physiotherapist, 74% improved their PFM contraction.
In a Norwegian study of primiparous women, only 4% were unable to contract at 6 weeks postpartum, but many of these women had been tested and taught a correct PFM contraction during pregnancy and the physiotherapist spent extra time with manual techniques at the first consultation. PFM strength and endurance were reduced by > 50% after vaginal birth, with significantly greater deficits for women with instrumental delivery. Primiparous postpartum women with major PFM injuries diagnosed by ultrasound had 47% weaker PFM than those without injury (MD 8 cmH2O, 95% CI 5 to 10).
Description of the Norwegian Pelvic Floor Muscle Group Training Concept
The Norwegian PFM group training protocol has two main stages.
Stage 1: Search, Find, Learn and Control
This important first stage is an individual consultation with a trained physiotherapist. After thorough teaching of the anatomy and physiology of the pelvic floor using anatomical models/drawings of the pelvis, the physiotherapist explains the function of the PFM and how it may prevent and treat SUI/mixed urinary incontinence and pelvic organ prolapse. The woman then tries to contract the PFM on her own and is allowed time to empty her bladder before assessment of her ability to contract the PFM. With the patient in a supine position with hips and knees bent, the woman tries to contract the PFM while the physiotherapist observes the perineum. The physiotherapist then inserts one finger at the lower third of the vagina and asks the patient to squeeze and lift around the finger. Feedback of performance of the contractions is given to the patient.
If the patient can perform a correct contraction, vaginal resting pressure and activity and muscle strength and endurance are measured, and the patient is referred to the exercise class.
Women who are unable to contract can feel that this is difficult to cope with, and the physiotherapist should explain that this is common, referring to studies finding that > 30% of women have been found to be unable to perform a correct contraction at their first consultation. When a woman is unable to contract (no visible or palpable contraction or straining), she is asked to try to contract at home on her own for a week with advice to stop the dribbling at the end of voiding (just as a test, not to be done as a training routine), and sit on an armrest or edge of a table with pressure towards the perineum or press her hand towards the perineum and try to lift away from the chair/hand. If she is still unable to contract at her second visit, the physiotherapist may use facilitation techniques (tapping, fast stretching, massage, electrical stimulation) in order to stimulate muscle function. Most women can learn to perform a correct PFM contraction, but there are some women who remain unable, and they will obviously not respond to PFMT. Furthermore, if women are straining or pushing down, PFMT theoretically can cause more damage, as straining is a risk factor for both SUI and pelvic organ prolapse.
Stage 2: Strength Training
The aim of the strength training program is to build up the muscles and improve structural support to counteract increased intra-abdominal pressure and ground reaction forces. Possible permanent changes to the PFM due to strength training are listed in Box 2. Such changes have been shown in an assessor-blinded randomised trial after 6 months of individualised and supervised PFMT following the same training principles.
Box 2
Possible Permanent Changes to the Pelvic Floor Muscles Due to Strength Training.
The above changes may lead to an automatic function of the pelvic floor with less opening of the levator hiatus and less downward movement of the pelvic floor during an increase in intra-abdominal pressure. In the group training class, strength training of the PFM is conducted in five different positions, with attempts of eight to twelve maximum voluntary contractions in each position. The participants are instructed to hold each contraction for 6 to 8 seconds. About half of the contractions in each position are ‘intensive contractions’ meaning that the women are asked to contract as hard as possible, hold the contraction for 6 to 8 seconds, and then try to add three to four fast contractions on top of the prolonged contraction. The physiotherapist uses strong verbal encouragement to motivate for effort of maximum voluntary contraction. In the clinical trials of this intervention, the patients have exercised in the class once a week. Positions with legs apart are used to avoid the strong outer pelvic muscles (hip adductor, gluteal and superficial abdominal muscles) taking over and masking attempts to contract the PFM. Small co-contractions of the inner abdominal muscles have always been allowed in this program because it does not seem to be possible to perform maximum PFM contractions without some co-contraction of the abdominals. However, this is just a small in drawing of the abdominal wall on top of the PFM contraction. In addition to the supervised group or individual training program, the patients are asked to perform three sets of eight to twelve maximum voluntary contractions per day at home and to report training adherence in a training diary. DVDs, videos and apps can be used to guide and help adherence and intensity of the PFM home training program. The Norwegian PFMT group training class also contains training for other parts of the body. These exercises (strength training of other muscle groups, relaxation, breathing exercises and stretching of the back, neck and shoulders) are conducted in the breaks between each of the five sets of eight to twelve PFM contractions, with no encouragement to simultaneously contract the PFM. Hence, these other exercises should not be confused with functional training. Functional training is defined as ‘training that consists of training for tasks of daily living and self-care activities (eg, squatting to train quadriceps and gluteal muscles). Functional PFM training is ‘training and exercises that incorporate a correct PFM contraction into activities of daily living such as lifting, transferring out of bed, or sneezing’. This implies that the patients must think about contraction of the PFM all day long. To date, there is no evidence that this becomes an automatic behaviour or that adding functional training on top of PFMT is more effective than an adequately dosed strength training program alone. Since strength training of the PFM has such good effect, a large sample size is needed to show any extra benefit of adding adjuncts such as biofeedback or other exercise modalities. As many women with UI withdraw from general exercise, low-impact activities (no running and jumping) are the basis of the other exercises in the group PFMT program. The exercises should be easy to conduct and make the women feel empowered and that they can enjoy participating. Any exercises can be chosen in the breaks between PFM contractions; this program emphasises strength training of the back, abdominals, thigh and arms, ergonomics and stretching and relaxation of the neck and shoulders. These other exercises have never been intended to have any training effect on the PFM. As confirmed by Kruger et al, possible co-contractions of the PFM via contractions of other muscles have minimal potential for a training effect of the PFM. In the Norwegian program the exercises between the sets of PFMT are performed to music. This implies that the physiotherapist must be skilled in music analyses and know how to build up a program following music. The class ends with a 15-minute conversation about effective exercise training and motivation strategies to adhere to the program. The physiotherapist acts as a mentor and encourages women to exchange experiences and stories about how to adhere to the program and improvement of the condition. Possible advantages and disadvantages of conducting PFMT in a group setting are listed in Box 3. An example program that has been used in randomised controlled trials is described in Table 1. Box 3 Possible advantages and disadvantages of group pelvic floor muscle training.
Table 1. Example of a pelvic floor muscle exercise class following the Norwegian pelvic floor muscle training model
PFMT = pelvic floor muscle training, Y = yes.
Future Directions for Research and Practice There is international consensus that PFMT has Level 1 evidence (recommendation A) that it is effective and should be first-line treatment for SUI and pelvic organ prolapse. Adding group training to individual home training is more effective than home training alone, and group training is not inferior to individual training if the patients receive thorough instruction and adequate assessment and feedback of their ability to perform a correct PFM contraction. Group PFMT is cost-effective and can include health and fitness information and other exercises. It can also be a strong motivator for women to increase their physical activity levels, thereby facilitating them to start and continue with more advanced exercise programs. Therefore, PFMT classes have potential additional benefits to the patient, physiotherapist and society. One of the biggest challenges today is implementation of evidence from randomised trials and systematic reviews into clinical physiotherapy practice. For UI, the profession can choose from effective protocols proven in high-quality randomised trials to guide practice. There is no evidence of any extra effect of adding other exercises (e.g. breathing or abdominal exercises) to PFMT for UI; the focus for evidence-based physiotherapy practice should therefore be on PFMT. There is still a need for randomised trials with high-quality methods and appropriate intervention protocols to investigate the effect of PFMT in the postpartum period for UI, pelvic organ prolapse and anal incontinence. Future research should focus on the effect of PFMT for women with perineal tears and major PFM injuries after birth trauma. In addition, randomised trials are required to explore the effects of different physiotherapy modalities to treat symptoms of overactive bladder, pelvic floor pain and sexual functions. More basic research on the pathophysiology and aetiology of all pelvic floor dysfunctions is needed. There is also a need for research on how to motivate the female population to increase their general physical activity levels and especially exercises for the PFM. More research should also investigate the barriers for including PFMT as a natural part of strength training programs for women in fitness centres and exercise classes.
References · https://www.sciencedirect.com/science/article/pii/S1836955320300655#bib52 · https://www.physio-pedia.com/Incontinence · https://www.medicalnewstoday.com/articles/165408#treatment |