Treatment Guidelines of The Upper Limb In Stroke Patients
Introduction
Reduced arm function causes a decrease of quality of life in stroke patients [1]. Initially, 85% of stroke patients have an impairment of arm-hand function. These impairments still exist in 55 to 75% of stroke patients after three to six months [2-4]. Six months after stroke 30-66% of stroke patients remain without voluntary function of the upper limb and 5-20% demonstrates complete recovery [2,5].
Walking and activities of daily living (ADL) seem to get more attention in order to optimize the opportunity for patients to be discharged home [6]. Therefore, intensive mobility training and early task oriented training with the affected arm may not be a priority [7,8], although recovery of function at all stages is possible [9]. The neural damage specifically involving the cortico-spinal tract reinforced with an emphasis on mobility, spontaneous preference to use the unaffected limb for independence in activities of daily living and the non-use of the affected upper limb may explain the limited and slower recovery of the dexterity of the upper limb. Apart from this, the early attention, which is given to gross motor skill, like walking and ADL functions, explains the difference in time of recovery after stroke. The attention often only shifts to upper limb treatment after some time. At this moment, not only the primary impairment, but also ‘learned non-use’ defines the probability of recovery.
There are various reasons why early implementation of upper limb rehabilitation is an important factor in the probability of recovery of upper limb function. After a stroke, the unaffected hemisphere inhibits the affected one [10,11]. This inter-hemispheric inhibition can be influenced by an early start of rehabilitation of the involved upper limb.
In order to keep the upper limb in the body scheme, early implementation of upper limb treatment is important. By involving the hand in treatment immediately post stroke reorganisation around the area of the stroke may be facilitated. The possible segmental competition may be affected [12]. Learning based therapy drives reorganisation of the brain maps. Early implement of hand use increases the probability of expanding the hand representation in the brain [13].
The prerequisites for recovery of voluntary selective movements of the upper limb in patients post stroke include good core stability, correct scapula setting, efficient scapular humeral rhythm, good somatosensory function and recovery of reach-related muscle function [14-16]. A dynamic, stabile trunk is the background for a proper function of shoulder muscles. The trunk must automatically anticipate upper limb movements by setting anticipatory postural adjustments (APA). APA’s provide a chain of fixation for prime movers [17] and are only effective if sufficient postural control, built on a stabile core, is present.
Scapula setting with proper alignment of the glenoid allows for the most efficient position of the rotator cuff muscles to function. This allows recruitment of the triceps brachii, which is considered to be a prime mover in a forward reaching task and a key muscle targeted by the reaching practice [18]. Simultaneous contractions of External rotators of the shoulder and triceps are important for efficient reach and grasp [19,20]. Selective recruitment of deltoideus, pars spinalis, and medial triceps are important conditions to set the of function in early rehabilitation of the upper limb.
Sensorimotor processing of the hand is critically important to restoring functional movements of the upper limb. That’s why early, specific and task-oriented hand therapy is important in the recovery of the upper limb.
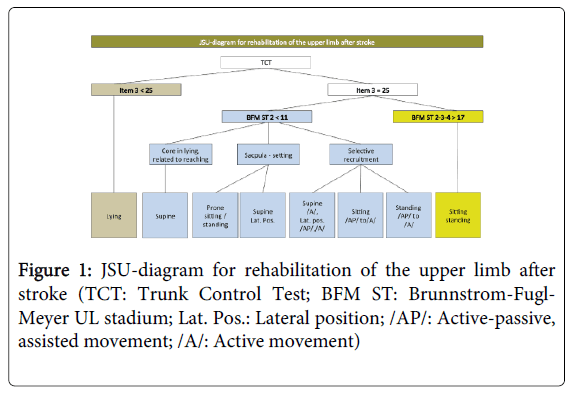
The JSU diagram (JSU: Jessa Sint-Ursula) has been proposed by Jessa Sint-Ursula as a model for rehabilitation of the upper limb after stroke (Figure 1). The JSU flow chart was developed by therapists of the Jessa - hospital, rehabilitation campus Sint-Ursula, Herk-de-Stad, Belgium, to shape the early, specific and task-oriented therapy of the upper limb.
Figure 1: JSU-diagram for rehabilitation of the upper limb after stroke (TCT: Trunk Control Test; BFM ST: Brunnstrom-Fugl- Meyer UL stadium; Lat. Pos.: Lateral position; /AP/: Active-passive, assisted movement; /A/: Active movement)
The JSU diagram should be considered a guideline to determine the objectives needed to shape the rehabilitation of various stages of recovery. The diagram starts with upper limb rehabilitation from day one, even in the absence of sufficient trunk control. To our knowledge, no structured model relating starting position to stage of recovery has been published.
JSU Diagram and ICF
The bio-psycho-social model of the ICF has been used as a frame of reference when designing the JSU-diagram. The JSU-diagram is based on test results of the Trunk Control Test [21] and the Brunnstrom-Fugl-Meyer upper limb assessment [22], which in turn are part of the clinical examination. The clinical examination starts from the goals of the patient, which are defined on the levels of activity and participation. The functional properties and quality of movement are assessed within the given activities. Therapists break eventual inefficiencies into disorders on the structure/function level. The therapist tries to influence these disorders by offering meaningful tasks. The patient thinks in terms of ‘activity’, the therapist keeps in mind the structure/function level. Progressively offering meaningful activities, which are practiced and reinforced can lead to neural adaptation of the brain.
Choice of Measurements: Trunk Control Test (TCT) and Brunnstrom Fugl-Meyer Test (BFM)
In the JSU-diagram, a first division is made, using item 3 of the Trunk Control Test. Item 3 (balance in sitting position on the edge of the bed with the feet off the ground for at least 30 seconds) distinguishes patients who can or cannot sit. If a patient is not able to sit (Item 3<25), the upper limb can be treated in lying (supine, side-lying on the involved or non involved side).
If the patient is able to sit independent (Item 3=25), the Brunnstrom Fugl-Meyer upper limb Test is used for decision making. The Brunnstrom Fugl-Meyer Test evaluates the movement of shoulder, elbow, wrist and hand and the coordination of the upper limb and discriminates between moving the arm in or out of flexion pattern. Abduction and internal rotation of the shoulder, and flexion of the elbow characterize moving the arm in flexion pattern. The Brunnstrom-Fugl-Meyer Test was chosen because it has prognostic properties for the recovery of dexterity [23-25].
A score <11 on stage 2 of BFM means that the patient is not able to move out of flexion pattern. A maximum score on the items related to shoulder movements (elevation, adduction, abduction, and internal rotation), results in a score of 10 points. A score<11 points means that there is a lack of selective movement. The patient moves his arm in a flexion pattern, and glenohumeral external rotation is difficult, if not impossible.
Possible causes of moving the arm in a flexion pattern relate to a lack of core stability, inadequate scapula setting and a lack of selective recruitment. It is the aim of this manuscript to address these issues in the various starting positions, which are described in the JSU diagram. For example, lying on the hemiplegic side can be chosen to stabilise the involved scapula in a passive way, which will make the external rotators of the shoulder more accessible. In this position, the flexor synergy may be influenced. The patient should be able to move out of the flexion pattern if the score on item 2-3-4 of the BFM exceeds 17. Selectivity of movement is possible and therefore task oriented practice in sitting and standing is preferable to treat reaching and grasping.
JSU Diagram
TCT item 3<25
The aim in this phase is early activation of the upper limb. A starting position is chosen in order of increasing difficulty. For example, the lateral position on the affected side may be the starting place, followed by supine position and then the lateral position on the non-affected side.
Lateral position on the affected side
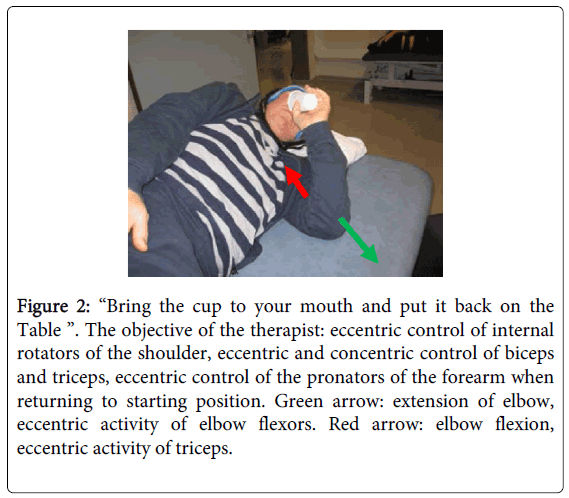
In this position, the trunk, scapula and upper arm are passively stabilized. The arm is positioned in 90° of ventral flexion, which mimics a reaching position. The patient has a lot of visual information about the position of the arm and hand and in lateral lying proprioceptive and sensory information increases (Figure 2).
Figure 2: “Bring the cup to your mouth and put it back on the Table ”. The objective of the therapist: eccentric control of internal rotators of the shoulder, eccentric and concentric control of biceps and triceps, eccentric control of the pronators of the forearm when returning to starting position. Green arrow: extension of elbow, eccentric activity of elbow flexors. Red arrow: elbow flexion, eccentric activity of triceps.
During therapy, the emphasis is put on eccentric movement of internal rotators of the shoulder and of pectoralis major, activation of biceps and triceps (concentric and eccentric). Movement control of pronators, palmar and dorsal flexors and finger muscles can be exercised, according to the capabilities of the patient. Grasping can be included to combine reaching and grasping even in this early phase of recovery.
When shaping the therapy, the therapist tries to choose a meaningful activity. Doing so, the therapist defines the aim on a function/structure level, whilst the patient is trying to solve a ‘motor problem’. Doing so, the patient is ‘thinking’ on an activity level.
Supine
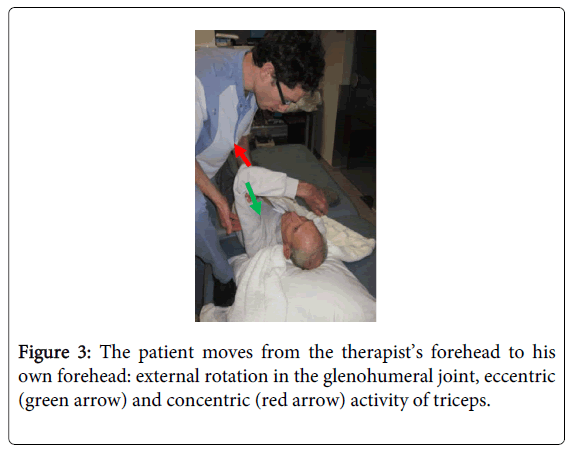
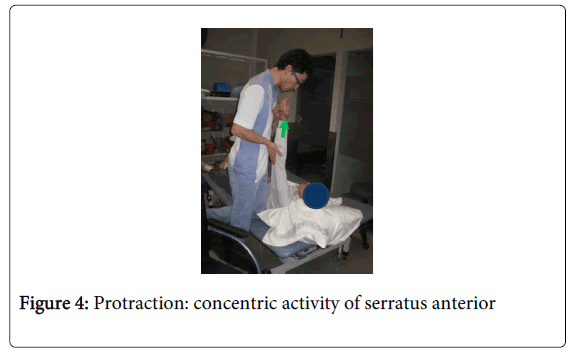
The passive stability of the trunk and scapula is preserved in supine. In this starting position however, the degrees of freedom of movements and the effect of gravity increase, making the task of moving the arm more difficult (Figures 3-5). For example, focus can be on eccentric and concentric activity of serratus anterior (scapula protraction/scapula setting), eccentric activity of pectoralis and deltoideus, pars anterior (horizontal abduction), concentric and eccentric activity of shoulder flexors (ventral flexion). Eccentric and concentric control of triceps can be addressed with the shoulder in ventral flexion (Figure 3).
Figure 3: The patient moves from the therapist’s forehead to his own forehead: external rotation in the glenohumeral joint, eccentric (green arrow) and concentric (red arrow) activity of triceps.
Figure 4: Protraction: concentric activity of serratus anterior
Figure 5: Functional task: "Follow the ring with the stick": eccentric activity of pectoralis major the internal rotator of the shoulder, concentric activity of triceps, supinators and wrist extensors.
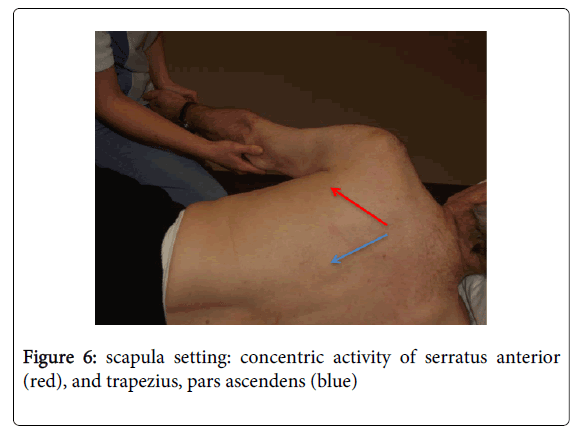
The relationship between core stability and scapula setting is best addressed in the lateral position on the non-affected side. Scapula setting can be exercised in preparation of reaching and grasping. The goal of therapy in this position is scapula setting, shoulder protraction (serratus anterior), concentric and eccentric control of external rotators of the shoulder and deltoideus, pars posterior, concentric and eccentric activity of triceps brachii. A task is chosen in which grasping is included. Finally, this position inhibits the non-affected side in case of over-activity (Figure 6).
Figure 6: scapula setting: concentric activity of serratus anterior (red), and trapezius, pars ascendens (blue)
Lateral position on the non-affected side
TCT Item 3=25, BFM UL Stage 2<11
At this stage, the main objective is practicing core stability in relation to reaching, scapula setting and selective recruitment of muscle activity.
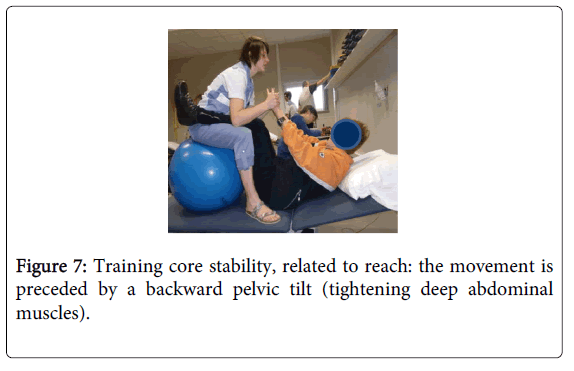
Core stability in supine, related to reaching
Adequate core stability gives an anchor point for scapula setting. In order to set the scapula, serratus anterior needs stable external oblique abdominals. In supine, core stability is trained by strengthening the deep abdominal musculature. Doing so, it is important to emphasize the relationship with reaching (Figure 7).
Figure 7: Training core stability, related to reach: the movement is preceded by a backward pelvic tilt (tightening deep abdominal muscles).
Scapula setting
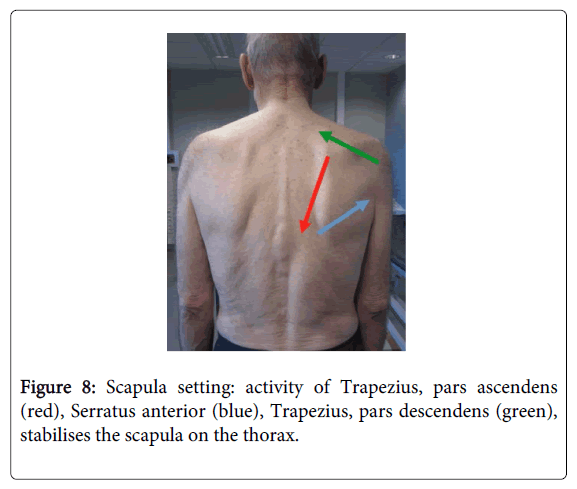
A lack of core stability and absence of adequate scapula setting are reasons for moving the upper limb in flexor pattern. As a result of this, and due to an inefficient selective movement, reaching is done with shoulder abduction, internal rotation and predominance of elbow flexion (Figure 8).
Figure 8: Scapula setting: activity of Trapezius, pars ascendens (red), Serratus anterior (blue), Trapezius, pars descendens (green), stabilises the scapula on the thorax.
When practicing scapula setting, a correct cooperation between trapezius, pars ascendens, serratus anterior, and trapezius, pars descendens and rhomboideï is essential (Figure 7). An inefficient scapula setting leads to insufficient exorotation of the humerus and to difficulties with elevation of the arm. In addition, the risk of impingement of the supraspinatus tendon increases because of poor scapulohumeral rhythm. Sufficient core stability and efficient scapula setting frees the arm and hand for selective movement.
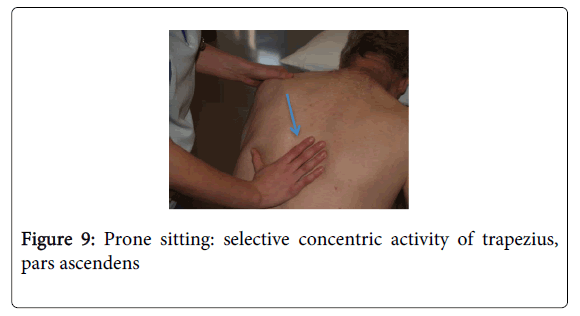
Analytical work with scapula is possible in prone sitting and prone standing. This position offers the possibility to work with the scapula on a stable trunk. The scapula is activated in the body scheme by tactile and proprioceptive stimulation. Selective movement (eccentric, isometric and concentric) of rhomboidei and trapezius, pars ascendens is facilitated (Figure 9). Too much activity of trapezius, pars descendens is inhibited. If an efficient scapula setting is achieved, brachiï can be addressed.
Figure 9: Prone sitting: selective concentric activity of trapezius, pars ascendens
Supine/lateral position
Scapula setting can be integrated within the activity level in supine. The number of degrees of freedom, which have to be controlled, increases in relation to the chosen starting position: lateral position on the affected side, supine, lateral position on the non-affected side.
Selective Recruitment
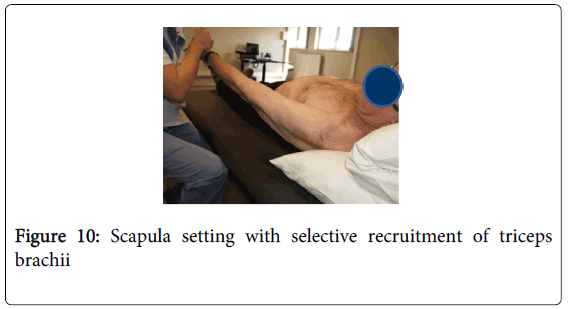
In this phase, selective movement is trained by giving functional tasks in various starting positions. Changing the environment and task offers a variety of situations in which motor learning becomes possible. The patient learns to move in the most efficient way, taking into account the remaining potential (Figure 10).
Figure 10: Scapula setting with selective recruitment of triceps brachii
Eventual starting postures are lateral position on affected side, supine, lateral position on non-affected side, sit and stand. Activities are shaped by the therapist to influence the function and structural level. In other words, the patient 'thinks’ activity; the therapist 'thinks' structure/function. A key issue is that the direction of articular movement can be different of the mentioned muscular activity (Figures 2 and 5)
Selective recruitment of deltoid, pars spinalis, triceps brachii, and wrist extensors is emphasized (Figure 11).
Figures 11: Functional activities
Limitations of this Analysis of Rehabilitation of the Upper Limb Post Stroke
This manuscript describes a potential paradigm for improving upper limb function post stroke. However, this is not an evidence-based review and it does not include a report of a clinical trial. While the proposed strategy for improving the recovery of function of the upper limb follows a logical theoretical strategy, there is no evidence-based review that specifically supports the recommendations.
The authors are aware that many factors will affect motor performance. The importance of for instance cognitive and emotional functions, speech functions, spasticity, post-stroke shoulder pain, balance and coordination, etc. shouldn’t be underestimated and have to be part of the clinical reasoning process, which is embedded within the JSU-Diagram and which leads to adequate treatment choices.
Conclusion
Recovery of efficient, functional use of the upper limb post stroke can contribute to an increased quality of life. After a stroke, the literature suggests immediate implementation of therapy for the upper limb may reduce the risk of secondary dysfunction related to non-use of the arm/hand. The JSU diagram offers a guideline for implementing upper limb treatment at various stages of recovery after stroke. Prerequisites for efficient voluntary reach and grasp skills require adequate postural control, core stability, scapula setting and selective recruitment of reach-related musculature. Objectives must be defined on an activity level. The choices of rehabilitation environment, task, starting positions and handling techniques may influence the maximum level of functional levels of voluntary movement recovery. Further research on the effectiveness of the treatment strategy, which is described in the JSU-diagram, is needed.
References
- Nichols-Larsen DS, Clark PC, Zeringue A, Greenspan A, Blanton S (2005) Factors influencing stroke survivors' quality of life during subacute recovery. Stroke 36: 1480-1484.
- Parker VM, Wade DT, Langton Hewer R (1986) Loss of arm function after stroke: measurement, frequency, and recovery. Int Rehabil Med 8: 69-73.
- Olsen TS (1990) Arm and leg paresis as outcome predictors in stroke rehabilitation. Stroke 21: 247-251.
- Feys HM, De Weerdt WJ, Selz BE, Cox GA, Spichiger R, et al. (1998) Effect of a Therapeutic Intervention for the Hemiplegic Upper Limb in the Acute Phase After Stroke : A Single-Blind, Randomized, Controlled Multicenter Trial. Stroke 29:785-792.
- Kwakkel G, Kollen BJ, van der Grond J, Prevo AJ (2003) Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke 34: 2181-2186.
- Tsu AP, Abrams GM1, Byl NN2 (2014) Poststroke upper limb recovery. SeminNeurol 34: 485-495.
- Barker RN, Brauer SG (2005) Upper limb recovery after stroke: the stroke survivors' perspective. DisabilRehabil 27: 1213-1223.
- Doyle SD, Bennett S, Dudgeon B (2014) Upper limb post-stroke sensory impairments: the survivor's experience. DisabilRehabil 36: 993-1000.
- Verheyden G, Nieuwboer A, De Wit L, Thijs V, Dobbelaere J, et al. (2008) Time course of trunk, arm, leg, and functional recovery after ischemic stroke. Neurorehabil Neural Repair 22: 173-179.
- Nowak DA, Grefkes C, Ameli M, Fink GR (2009) Interhemispheric competition after stroke: brain stimulation to enhance recovery of function of the affected hand. Neurorehabil Neural Repair 23: 641-656.
- Takeuchi N, Tada T, Toshima M, Matsuo Y, Ikoma K (2009) Repetitive transcranial magnetic stimulation over bilateral hemispheres enhances motor function and training effect of paretic hand in patients after stroke. J Rehabil Med 41: 1049-1054.
- Merians AS, Tunik E, Fluet GG, Qiu Q, Adamovich SV (2009) Innovative approaches to the rehabilitation of upper extremity hemiparesis using virtual environments. Eur J PhysRehabil Med 45: 123-133.
- Oujamaa L, Relave I, Froger J, Mottet D, Pelissier JY (2009) Rehabilitation of arm function after stroke. Literature review. Ann PhysRehabil Med 52: 269-293.
- Aimola E, Santello M, La Grua G, Casabona A (2011) Anticipatory postural adjustments in reach-to-grasp: effect of object mass predictability. NeurosciLett 502: 84-88.
- Kisiel-Sajewicz K, Fang Y, Hrovat K, Yue GH, Siemionow V, et al. (2011)Weakening of Synergist Muscle Coupling During Reaching Movement in Stroke Patients. Neurorehab and neural repair 25: 359-368
- Barker RN, Brauer S, Carson R (2009) Training-induced changes in the pattern of triceps to biceps activation during reaching tasks after chronic and severe stroke. Exp Brain Res 196: 483-496.
- Caronni A, Cavallari P (2009) Anticipatory postural adjustments stabilise the whole upper-limb prior to a gentle index finger tap. Exp Brain Res 194: 59-66.
- Harris-Love ML, Morton SM, Perez MA, Cohen LG, (2011) Mechanism of short-term training-induced reaching improvement in severely hemiparetic stroke patients: a TMS study. Neurorehabilitation and Neural Repair 25: 398-411.
- Kibler WB, Sciascia A, Wilkes T (2012) Scapular dyskinesis and its relation to shoulder injury. J Am AcadOrthopSurg 20: 364-372.
- Mottram SL, Woledge RC, Morrissey D (2009) Motion analysis study of a scapular orientation exercise and subjects' ability to learn the exercise. Man Ther 14: 13-18.
- Collin C, Wade D (1990) Assessing motor impairment after stroke: a pilot reliability study. J NeurolNeurosurg Psychiatry 53: 576-579.
- Gladstone DJ, Danells CJ, Black SE (2002) "The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties." Neurorehabilitation and neural repair 16: 232-240.
- Barr KP, Griggs M, Cadby T (2005) Lumbar stabilization: core concepts and current literature, Part 1. Am J Phys Med Rehabil 84: 473-480.
- Isa T, Ohki Y, Alstermark B, Pettersson LG, Sasaki S (2007) Direct and indirect cortico-motoneuronal pathways and control of hand/arm movements. Physiology (Bethesda) 22: 145-152.
- Rathelot JA, Strick PL (2009) Subdivisions of primary motor cortex based on cortico-motoneuronal cells. ProcNatlAcadSci U S A 106: 918-923.
http://www.optimaphysio.com/blog/treatment-guideline-of-the-upper-limb-in-stroke-patients